Multivariable linear model for predicting graft weight based on 3-dimensional volumetry in regards to body weight change of liv
Purpose: The purpose of this study is to build a prediction model for estimating graft weight about different graft volumetry methods combined with other variables. Methods: Donors who underwent living-donor right hepatectomy from March 2021 to March 2023 were included. Estimated graft volume measured by conventional method and 3-dimensional (3D) software were collected as well as the actual graft weight. Linear regression was used to build a prediction model. Donor groups were divided according to the 3D volumetry of <700 cm3, 700–899 cm3, and ≥900 cm3 to compare the performance of different models. Results: A total of 119 donors were included. Conventional volumetry showed R2 of 0.656 (P < 0.001) while 3D software showed R2 of 0.776 (P < 0.001). The R2 of the multivariable model was 0.842 (P < 0.001) including for 3D volume (β = 0.623, P < 0.001), body mass index (β = 7.648, P < 0.001), and amount of weight loss (β = –7.252, P < 0.001). The median errors between different models and actual graft weight did not differ in donor groups (<700 and 700–899 cm3), while the median error of univariable linear model using 3D software (122.5; interquartile range [IQR], 61.5–179.8) was significantly higher than multivariable-adjusted linear model (41.5; IQR, 24.8–69.8; P = 0.003) in donors with estimated graft weight ≥900 cm3. Conclusion: The univariable 3D volumetry model showed an acceptable outcome for donors with an estimated graft volume <900 cm3. For donors with an estimated graft volume ≥900 cm3, the multivariable-adjusted linear model showed higher accuracy. [Ann Surg Treat Res 2024;107(2):91-99] English: 3D modeling enhances surgical precision by: Providing detailed anatomical insights for preoperative planning. Reducing human errors in volumetric assessments. Supporting personalized, data-driven surgical strategies, especially in challenging cases like large-volume liver grafts. Korean: 3D 모델링은 수술 계획을 다음과 같이 개선합니다: 수술 전 계획을 위한 세밀한 해부학적 정보를 제공합니다. 용적 평가에서 인간 오류를 줄입니다. 특히 대용량 간 이식과 같은 복잡한 사례에서 맞춤형 데이터 기반 수술 전략을 지원합니다.
Author jsrrules
Date 2024.12.08

Risk Factors Associated With Surgical Morbidities of Laparoscopic Living Liver Donors
Objective: This study analyzed the incidence and risk factors for surgical morbidities of laparoscopic living donors. Background: Although laparoscopic living donor programs have been established safely in leading centers, donor morbidities have not been discussed sufficiently. Methods: Laparoscopic living donors operated on from May 2013 to June 2022 were reviewed. Donor complications were reviewed, and factors related to bile leakage and biliary stricture were analyzed using the multivariable logistic regression method. Results: A total of 636 donors underwent laparoscopic living donor hepatectomy. The open conversion rate was 1.6%, and the 30-day complication rate was 16.8% (n=107). Grade IIIa and IIIb complications occurred in 4.4% (n=28) and 1.9% (n=12) of patients, respectively. The most common complication was bleeding (n=38, 6.0%). Fourteen donors (2.2%) required reoperation. Portal vein stricture, bile leakage, and biliary stricture occurred in 0.6% (n=4), 3.3% (n=21), and 1.6% (n=10) of cases, respectively. The readmission rate and reoperation rate were 5.2% (n=33) and 2.2% (n=14), respectively. Risk factors related to bile leakage were 2 hepatic arteries in the liver graft (OR=13.836, CI=4.092–46.789, P<0.001), division-free margin<5 mm from the main duct (OR=2.624, CI=1.030–6.686, P=0.043), and estimated blood loss during operation (OR=1.002, CI=1.001–1.003, P=0.008), while the Pringle maneuver (OR=0.300, CI=0.110–0.817, P=0.018) was protective against leakage. Regarding biliary stricture, bile leakage was the only significant factor (OR=11.902, CI=2.773–51.083, P=0.001). Conclusions: Laparoscopic living donor surgery showed excellent safety for the majority of donors, and critical complications were resolved with proper management. To minimize bile leakage, cautious surgical manipulation is needed for donors with complex hilar anatomy. This study analyzed risk factors and incidence rates of surgical morbidities in laparoscopic living donor hepatectomy (LLDH) performed over a 9-year period, focusing on complications like bile leakage, biliary stricture, and portal vein stricture. Key Findings: Patient Cohort: Total donors: 636. Open conversion rate: 1.6%. Overall complication rate: 16.8%. Severe complications (Clavien-Dindo grade ≥III): 6.3%. Portal vein stricture: 0.6%, all resolved with intervention. Bile leakage: 3.3%, often associated with complex bile duct and hepatic artery anatomy. Biliary stricture: 1.6%, all managed successfully. Risk Factors: Bile Leakage: Two hepatic arteries in the graft (OR: 13.836; P < 0.001). Division-free margin <5 mm from the main duct (OR: 2.624; P = 0.043). Higher estimated blood loss (OR: 1.002; P = 0.008). Use of the Pringle maneuver was protective (OR: 0.300; P = 0.018). Biliary Stricture: Strongly linked to prior bile leakage (OR: 11.902; P = 0.001). Key Outcomes: Comprehensive complication index median: 0. Most complications were successfully resolved with minimal long-term morbidity. Conclusion: LLDH demonstrates excellent safety when performed by experienced teams. Detailed preoperative imaging and cautious surgical planning are critical to minimizing donor risks, particularly for cases with complex hilar anatomy. 3D modeling and imaging technologies are critical for ensuring safe laparoscopic donor hepatectomy: Enhanced Preoperative Planning: Visualizing vascular and bile duct anatomy minimizes risks of complications. Precision in Complex Cases: Detailed anatomical insights are essential for handling variations in hepatic arteries and bile ducts. Improved Donor Outcomes: Structured imaging reduces intraoperative risks, particularly for bile leakage and biliary stricture. 9년간 시행된 **복강경 생체 간 공여자 절제술(LLDH)**에서 발생한 수술 합병증의 발생률과 위험 요인을 분석하였습니다. 주요 합병증으로는 담즙 누출, 담관 협착, 문맥 협착 등이 포함되었습니다. 주요 결과: 환자군: 총 공여자: 636명. 개복 전환율: 1.6%. 전체 합병증 발생률: 16.8%. 중증 합병증(Clavien-Dindo 등급 ≥III): 6.3%. 문맥 협착: 0.6%, 모두 중재술로 해결. 담즙 누출: 3.3%, 복잡한 담관 및 간동맥 해부학과 연관. 담관 협착: 1.6%, 모두 성공적으로 관리. 위험 요인: 담즙 누출: 간동맥 2개가 포함된 이식편(OR: 13.836; P < 0.001). 주간관에서 5 mm 미만의 여유 분리 거리(OR: 2.624; P = 0.043). 수술 중 출혈량 증가(OR: 1.002; P = 0.008). Pringle 수기 사용은 보호적 역할(OR: 0.300; P = 0.018). 담관 협착: 이전 담즙 누출과 강한 연관성(OR: 11.902; P = 0.001). 주요 결과: 합병증 지수 중앙값: 0. 대부분의 합병증이 장기적 영향을 최소화하며 성공적으로 해결됨. 결론: LLDH는 경험이 풍부한 팀이 시행할 경우 우수한 안전성을 보입니다. 복잡한 간문부 해부학을 가진 경우, 세밀한 수술 계획과 철저한 사전 영상 검토가 공여자 위험을 최소화하는 데 중요합니다. 3D 모델링 및 영상 기술은 복강경 공여자 절제술의 안전성을 보장하는 데 필수적입니다: 수술 전 계획 강화: 혈관 및 담관 해부학을 시각화하여 합병증 위험을 최소화합니다. 복잡한 경우 정밀성: 간동맥 및 담관 변이를 처리하는 데 세부 해부학적 통찰이 필수적입니다. 공여자 결과 개선: 구조화된 영상은 특히 담즙 누출 및 담관 협착과 관련된 수술 중 위험을 줄여줍니다.
Author jsrrules
Date 2024.12.08
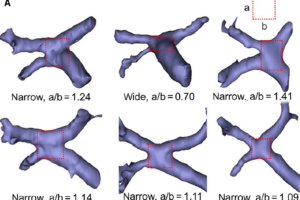
Laparoscopic Living Donor Right Hepatectomy Regarding the Anatomical Variation of the Portal Vein: A Propensity Score–Matched A
This study is designed to analyze the feasibility of laparoscopic living donor right hemihepatectomy in living donors with portal vein variation. Living donor liver transplantation cases using a right liver graft during the period of January 2014 to September 2019 were included. Computed tomographic angiographies of the donor were 3-dimensionally reconstructed, and the anatomical variation of the portal vein was classified. To reduce selection bias, a 1:1 ratio propensity score–matched analysis between the laparoscopy group and the open group was performed. Surgical and recovery-related outcomes as well as portal vein complication-free survival, graft survival, and overall survival rates were analyzed. After matching, 171 cases in each group from 444 original cases were compared. The laparoscopy group had a shorter operation time (P < 0.001), a smaller number of additional opioids required by the donor (P < 0.001), and a shorter hospital stay (P < 0.001). There were no differences in the portal vein complication-free survival (P = 0.16), graft survival (P = 0.26), or overall survival rates (P = 0.53). Although portal vein complication-free survival was inferior in portal veins other than type I (P = 0.01), the laparoscopy group showed similar portal vein complication-free survival regardless of the anatomical variation of portal vein (P = 0.35 in type I and P = 0.30 in other types). Laparoscopic living donor right hemihepatectomy can be performed as safely as open surgery regardless of the anatomical variation of the portal vein. Study Focus: The study evaluates the feasibility and safety of laparoscopic living donor right hepatectomy (LLDRH) in cases with portal vein (PV) anatomical variations, using propensity score (PS)–matched analysis to compare laparoscopic and open surgery approaches. Key Findings: - Portal Vein Variations: PV variations (types II and III) were associated with more grafts having two PV openings, but laparoscopic surgery managed these safely with outcomes comparable to open surgery. Complication rates were similar between laparoscopy and open surgery regardless of PV type. - Safety and Efficiency: Laparoscopic surgery had shorter operation times, less blood loss, shorter hospital stays, and reduced opioid requirements compared to open surgery. Postoperative PV complication rates requiring intervention were lower in the laparoscopy group (1.8% vs. 7.0%, P = 0.03). - 3D Modeling: Preoperative 3D reconstructions of donor PV anatomy aided in surgical planning, especially for complex PV types, improving precision and safety. Conclusion: LLDRH is a safe and effective alternative to open surgery, even in cases with challenging PV variations, provided the surgical team has sufficient expertise. 3D modeling in laparoscopic liver surgery is pivotal for visualizing complex PV anatomy, improving preoperative planning, and enhancing surgical safety and precision. By reducing complications and streamlining procedures, 3D modeling facilitates the broader adoption of minimally invasive techniques in liver transplantation. 연구 초점: 이 연구는 문맥(portal vein, PV) 해부학적 변이를 가진 생체 공여자 간 우엽 절제술에서 복강경 수술의 안전성과 타당성을 평가하기 위해 성향 점수(PS) 매칭 분석을 사용하여 복강경 수술과 개복 수술을 비교했습니다. 주요 결과: - 문맥 변이: PV 변이(II형 및 III형)는 두 개의 문맥 개구부를 가지는 경우가 더 많았지만, 복강경 수술에서도 안전하게 관리되어 개복 수술과 유사한 결과를 보였습니다. PV 변이 유형에 관계없이 복강경과 개복 수술 간 합병증 비율은 유사했습니다. - 안전성과 효율성: 복강경 수술은 개복 수술에 비해 수술 시간 단축, 출혈량 감소, 입원 기간 단축, 진통제 요구량 감소 등의 장점을 보였습니다. 수술 후 문맥 합병증 발생률은 복강경 그룹에서 더 낮았습니다(1.8% vs. 7.0%, P = 0.03). - 3D 모델링: 공여자의 PV 해부학적 구조를 3D 재구성하여 복잡한 PV 유형에서도 수술 계획을 개선하고 정밀도와 안전성을 높였습니다. 결론: 충분한 경험을 가진 외과 팀이 수행한다면, 복강경 생체 공여자 간 우엽 절제술은 어려운 PV 변이를 가진 경우에도 안전하고 효과적인 대안으로 자리 잡을 수 있습니다. 복강경 간 수술에서 3D 모델링은 복잡한 문맥 해부학을 시각화하고, 수술 전 계획을 개선하며, 수술 안전성과 정밀성을 높이는 데 중요한 역할을 합니다. 합병증을 줄이고 절차를 간소화함으로써, 3D 모델링은 간 이식에서 최소 침습 기술의 광범위한 채택을 촉진합니다.
Author jsrrules
Date 2024.12.08
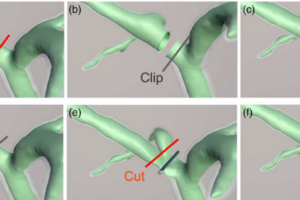
A Novel Technique for Bile Duct Division During Laparoscopic Living Donor Hepatectomy to Overcome Biliary Complications in Live
Background. This study was designed to analyze the clinical impact of a new bile duct division technique during laparoscopic living donor hepatectomy. Methods. Laparoscopic donor right hepatectomies performed by a single surgeon between December 2016 and August 2019 were included. Magnetic resonance cholangiopancreatography of the donors was reconstructed, and the length of the common channel of the dividing intrahepatic duct was measured. Patients were divided into 2 groups based on the bile duct division techniques of “clip and cut” versus “cut and clip.” Outcome of bile duct division was categorized based on the graft and bile duct type and number of bile duct openings. Results. A total of 147 transplantations were included. Outcomes in the “cut and clip” group were better than those in the “clip and cut” group with regard to obtaining an adequate division point (94.2% versus 78.8%; P = 0.019). The “cut and clip” showed superior biliary stricture-free survival than the “clip and cut” group (hazard ratio [HR], 0.456; confidence interval [CI], 0.217-0.957; P = 0.038) whereas recipients with hepaticojejunostomy (HR, 3.358; CI, 1.090-10.350; P = 0.035) and bile duct type other than type I (HR, 2.214; CI, 1.143-4.289; P = 0.018) showed increased risk for biliary stricture-free survival. Better outcome in terms of obtaining a single opening was also obtained in the “cut and clip” group (68.2% versus 84.6%; P = 0.040), and this difference was significant especially with a common channel shorter than 10 mm (45.5% versus 81.2%; P = 0.043). Conclusions. The “cut and clip” technique showed superior outcomes to the “clip and cut” technique in terms of fewer bile duct openings and biliary stricture-free survival of the recipients. This study introduces a novel bile duct division technique, “cut and clip,” for laparoscopic living donor hepatectomy (LLDH) and evaluates its effectiveness using 3D modeling for preoperative planning. The study analyzed outcomes from 144 cases performed between 2016 and 2019, comparing the “cut and clip” technique to the traditional “clip and cut” approach. Key Findings: - Improved Outcomes: The “cut and clip” technique resulted in fewer bile duct openings (15.4% vs. 31.8%) and significantly reduced biliary stricture rates in recipients. - Efficiency: Operation times were shorter in the “cut and clip” group (225.9 vs. 258.8 minutes, p < 0.001). - Enhanced Planning: 3D modeling based on MRCP enabled precise visualization of biliary structures and optimized division points. - Safety: The technique maintained donor safety while improving recipient outcomes. - Conclusion: The integration of 3D modeling and the “cut and clip” technique enhances surgical precision, reduces complications, and improves outcomes in LLDH, making it a safer and more efficient approach. 3D modeling technology is transforming surgical planning by providing detailed, patient-specific visualizations of complex anatomical structures. In LLDH, it enhances the precision of bile duct division, reduces complications, and optimizes surgical outcomes. As 3D modeling becomes more accessible, it is poised to set new standards in minimally invasive surgeries. 이 연구는 복강경 생체 간 기증자 간 절제술(LLDH)을 위한 새로운 담관 절단 기술인 “절단 후 클립(cut and clip)”을 도입하고, 수술 전 계획을 위한 3D 모델링을 활용하여 그 효과를 평가하였습니다. 2016년부터 2019년까지 수행된 144건의 사례를 분석하여 기존의 “클립 후 절단(clip and cut)” 방식과 비교하였습니다. 주요 결과: - 개선된 결과: “절단 후 클립” 기법은 담관 개구 수를 줄였고(15.4% vs. 31.8%), 수혜자의 담관 협착 비율을 유의미하게 감소시켰습니다. - 효율성: 수술 시간이 단축되었습니다(225.9분 vs. 258.8분, p < 0.001). - 계획 강화: MRCP를 기반으로 한 3D 모델링이 담관 구조를 정확하게 시각화하고 최적의 절단 지점을 결정하는 데 도움을 주었습니다. - 안전성: 기증자의 안전성을 유지하면서 수혜자 결과를 개선했습니다. 결론: 3D 모델링과 “절단 후 클립” 기술의 통합은 수술의 정밀도를 높이고 합병증을 줄이며 LLDH에서 더 안전하고 효율적인 접근 방식을 제공합니다. 3D 모델링 기술은 복잡한 해부학적 구조를 상세히 시각화하여 수술 계획을 혁신하고 있습니다. LLDH에서 담관 절단의 정밀도를 높이고 합병증을 줄이며 수술 결과를 최적화합니다. 3D 모델링의 접근성이 증가함에 따라 최소 침습 수술의 새로운 기준을 제시할 가능성이 큽니다.
Author jsrrules
Date 2024.12.08

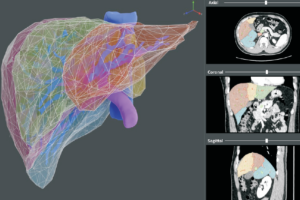
Image guidance using two-dimensional illustrations and threedimensional modeling of donor anatomy during living donor hepatecto
Abstract Background: For living donor liver transplantation, preoperative imaging is required for the safety of both the donor and the recipient. We previously initiated our image guidance program using two-dimensional illustrations and three-dimensional modeling in September 2018; herein, we analyzed the resultant changes in the clinical outcomes. Methods: Living donors and recipients who underwent liver transplantation between September 2017 and August 2019 were included. Cases with image guidance were compared to those without image guidance regarding the operative outcome, especially bile-duct opening in the graft as well as surgical complications. Results: Among 200 living donor transplantation, 90 transplantations were completed with image guidance. The image-guidance group had a higher rate of laparoscopy (80.9% vs. 97.8%; p < .001) as compared with the group without image guidance. Although there was no difference in the type of bile duct (p = .144), more grafts with single bile-duct openings were found in the image-guidance group (52.7% vs. 80.0%; p = .001). Consequently, achievements in bile-duct openings were superior in the image-guidance group (p = .022). There were no differences in bile leakage, graft failure, or number of deaths during the first month post-transplantation. Conclusion: As we initiated our image-guidance program for living donor liver transplantation, clinical outcomes, especially bile-duct division, were improved relative to before implementation. This study evaluates the impact of 2D illustrations and 3D modeling technology on living donor liver transplantation (LDLT) outcomes. A comparison was made between surgeries conducted before and after implementing an image-guidance program that utilized advanced 3D modeling techniques. Key Findings: - Improved Outcomes: The image-guidance group achieved superior bile-duct opening results (80.0% single openings vs. 52.7% in the non-image-guidance group, p = 0.001). - Efficiency Gains: Operation times were significantly reduced in the image-guidance group (240.3 ± 34.4 minutes vs. 259.8 ± 47.3 minutes, p = 0.002). - Enhanced Surgical Planning: 3D models provided detailed visualization of vascular and biliary structures, offering better guidance during donor hepatectomy. - Safety: There were no differences in post-operative complications or graft failure rates between the two groups. - Conclusion: The introduction of 3D modeling improved surgical precision, reduced operation times, and enhanced safety in laparoscopic donor liver transplantation. 3D modeling technology revolutionizes surgical planning and execution by offering precise, patient-specific visualizations of anatomical structures. In LDLT, it enhances safety, optimizes bile-duct division, and reduces operation times. This innovation represents a pivotal advancement in minimally invasive surgeries, supporting better outcomes and expanding the scope of laparoscopic procedures. 이 연구는 2D 일러스트레이션과 3D 모델링 기술이 생체 간 이식(LDLT) 결과에 미친 영향을 평가하였습니다. 첨단 3D 모델링 기술을 활용한 영상 유도 프로그램 도입 전후의 수술을 비교하였습니다. 주요 결과: - 결과 개선: 영상 유도 그룹에서 단일 담관 개구 비율이 더 높았음 (80.0% vs. 52.7%, p = 0.001). - 효율성 향상: 영상 유도 그룹의 수술 시간이 유의미하게 단축됨 (240.3 ± 34.4분 vs. 259.8 ± 47.3분, p = 0.002). - 수술 계획 강화: 3D 모델은 혈관 및 담관 구조를 상세히 시각화하여 수술 중 지침으로 작용. - 안전성 보장: 두 그룹 간 수술 후 합병증 및 이식 실패율에는 차이가 없었음. - 결론: 3D 모델링 기술 도입은 수술의 정밀도를 높이고 수술 시간을 단축하며 생체 간 이식의 안전성을 강화하였습니다. 3D 모델링 기술은 해부학적 구조를 정확하고 환자 맞춤형으로 시각화하여 수술 계획과 실행을 혁신합니다. 생체 간 이식에서 안전성을 높이고 담관 분리를 최적화하며 수술 시간을 단축합니다. 이러한 혁신은 최소 침습 수술의 결과를 개선하고 복강경 수술의 범위를 확장하는 중요한 진전을 나타냅니다.

